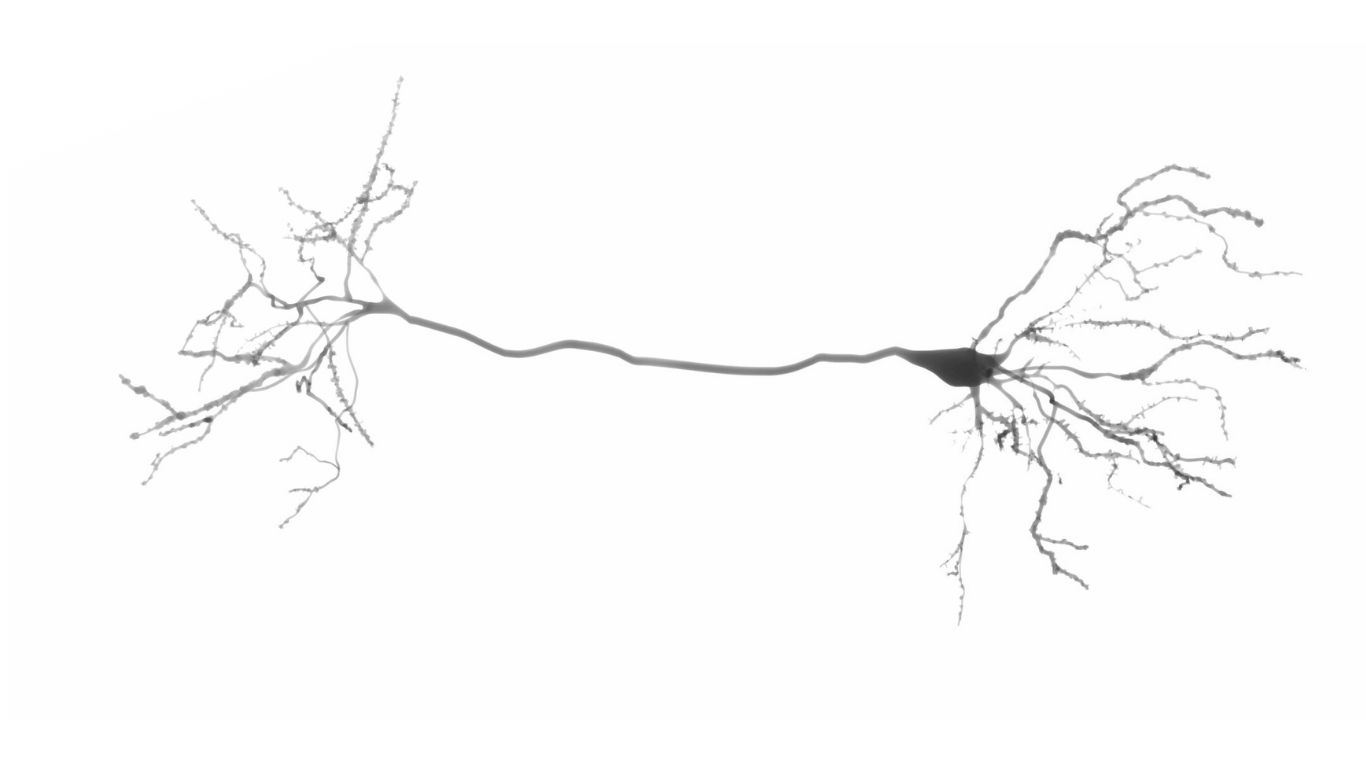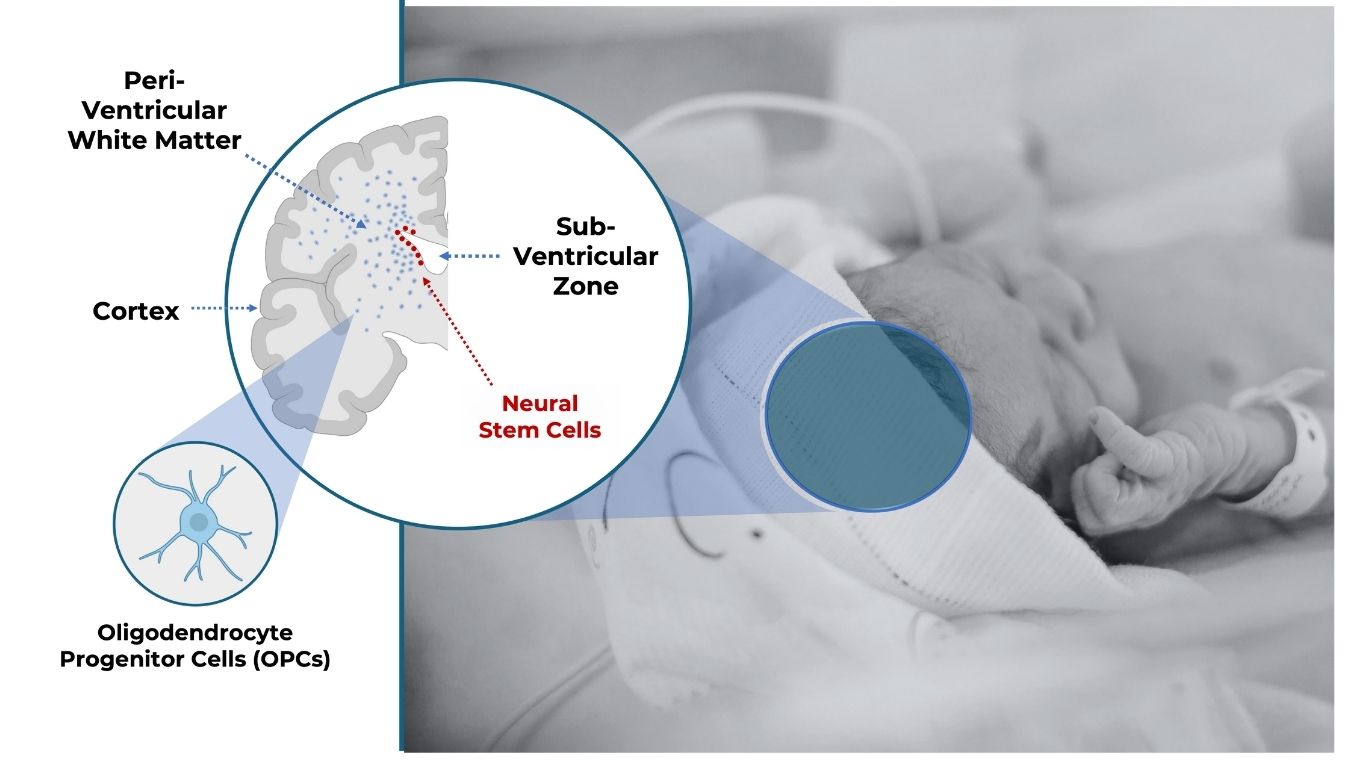
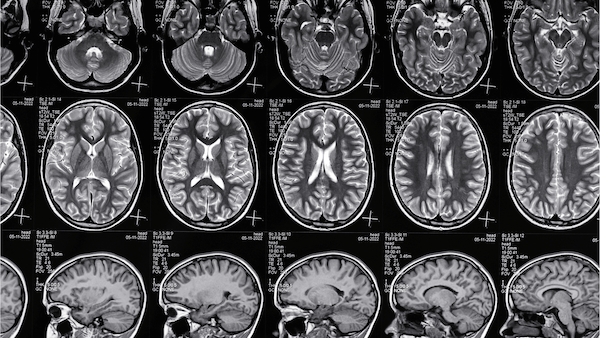
White Matter Injury (WMI)
is the most common brain injury in preterm infants. It is caused by inflammation and hypoxia, and leads to the loss of Oligodendrocyte Progenitor Cells (OPCs). This, in turn, disrupts myelination in the developing infant brain, and causes permanent motor and cognitive deficits - exemplified in severe cases by cerebral palsy.
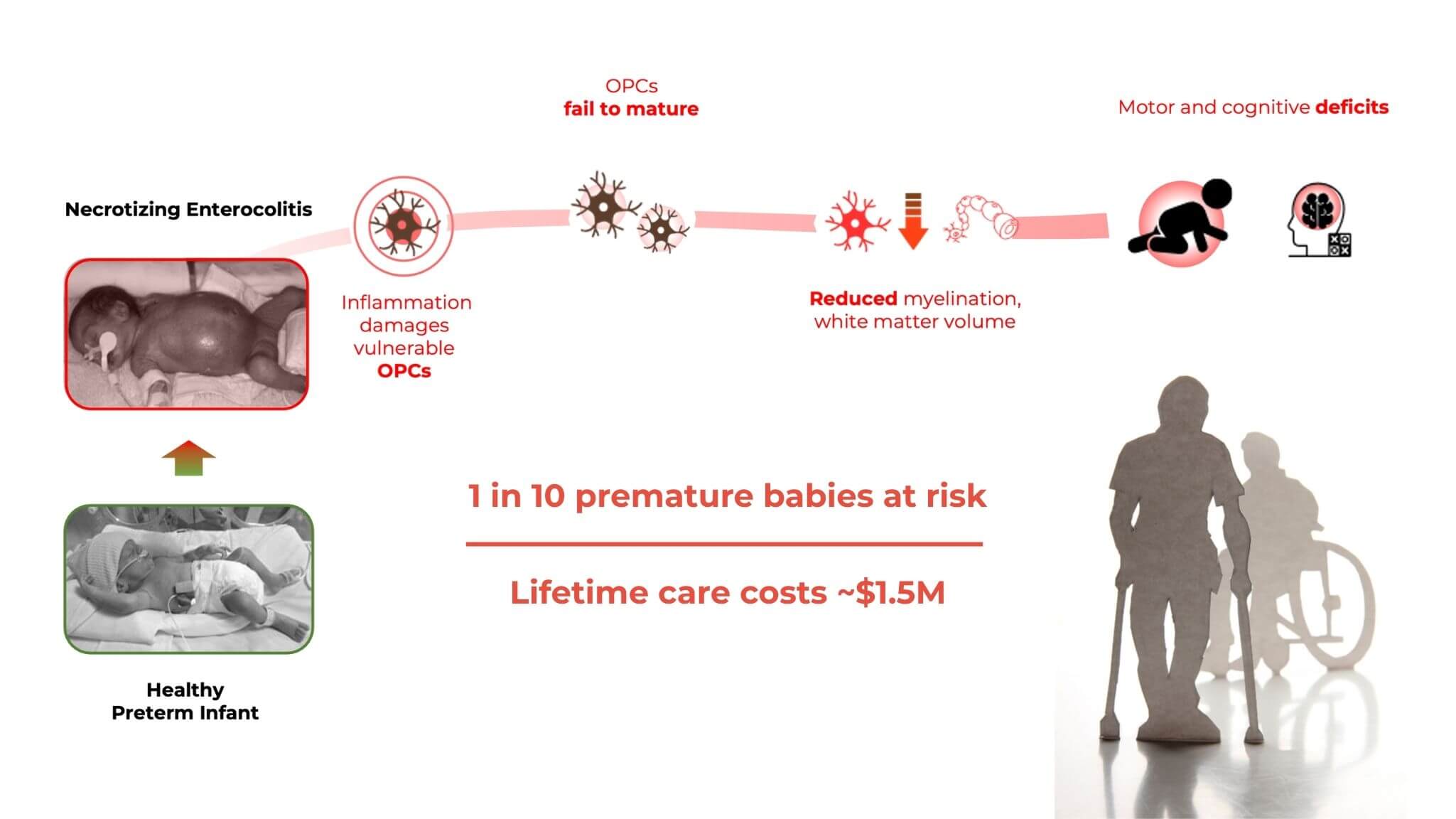
No Treatment, Lifelong Impact
Around 1 in 10 babies are born prematurely and at-risk for WMI. Yet there is currently no treatment available. Affected children face a lifetime of physical and cognitive disability, while parents face care costs of over $1.5M per child.
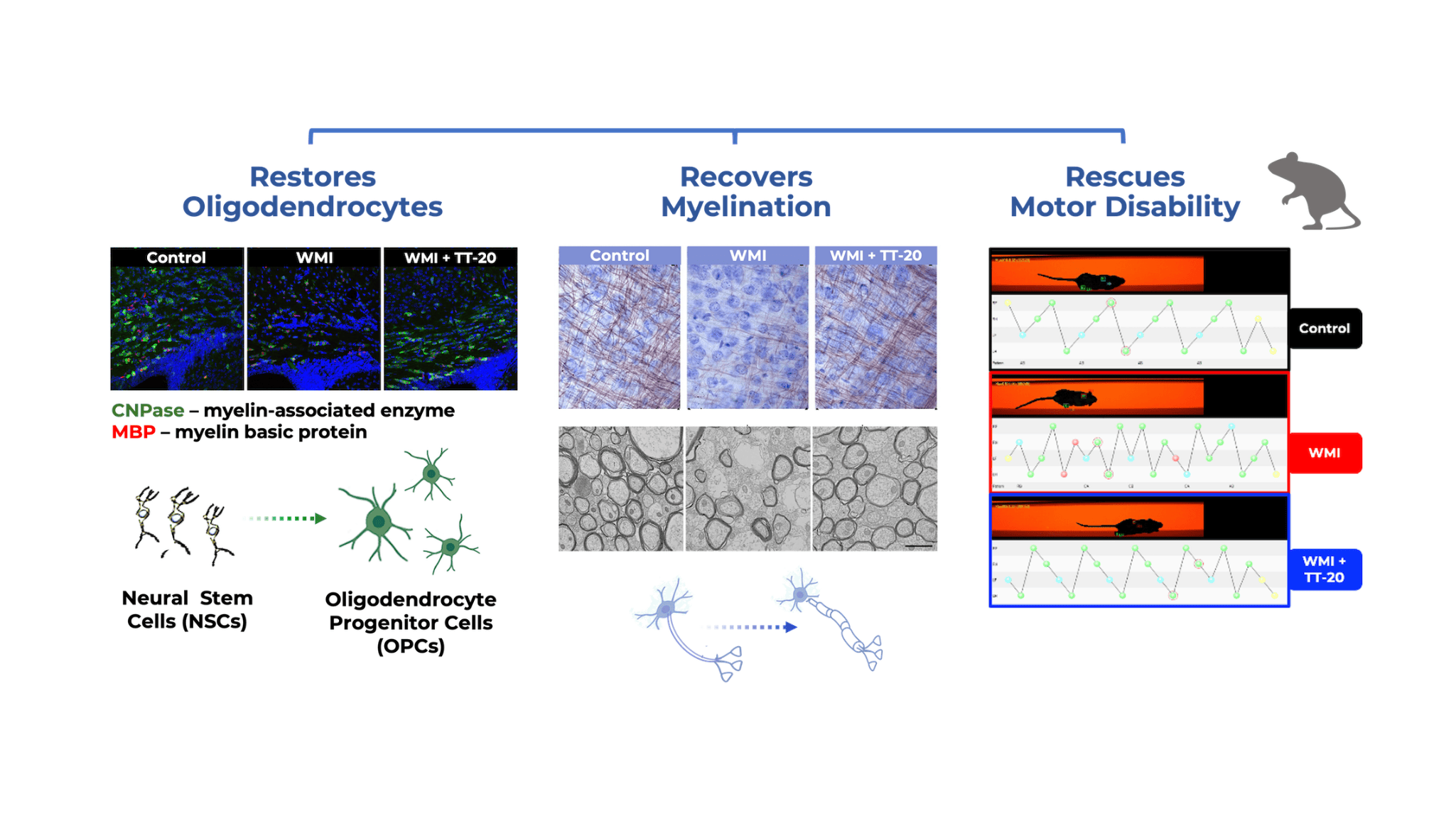
Nature Presents a Solution
Scientists at Duke University and TellusTx have discovered a family of compounds in maternal breast milk that stimulate Neural Stem Cells, restore OPC levels, and promote myelination - effectively restoring lost motor function after brain injury in neonatal animal models (see Chao, Benner et al. in References)

New Hope for the NICU
Tellus is set to take one such compound, TT-20, into human clinical trials. If successful, TT-20 will be the first treatment for WMI, to the benefit of patients and clinicians in Neonatal Intensive Care Units (NICUs) worldwide.
Future Applications
Promising new research suggests that oxysterol compounds similar to TT-20 could show great benefit in treating neonatal conditions beyond White Matter Injury, along with adult de-myelinating and neuro-inflammatory conditions such as multiple sclerosis.